Final Days: 10% Off Select Medical and Lab Equipment Ends July 31st, 2024
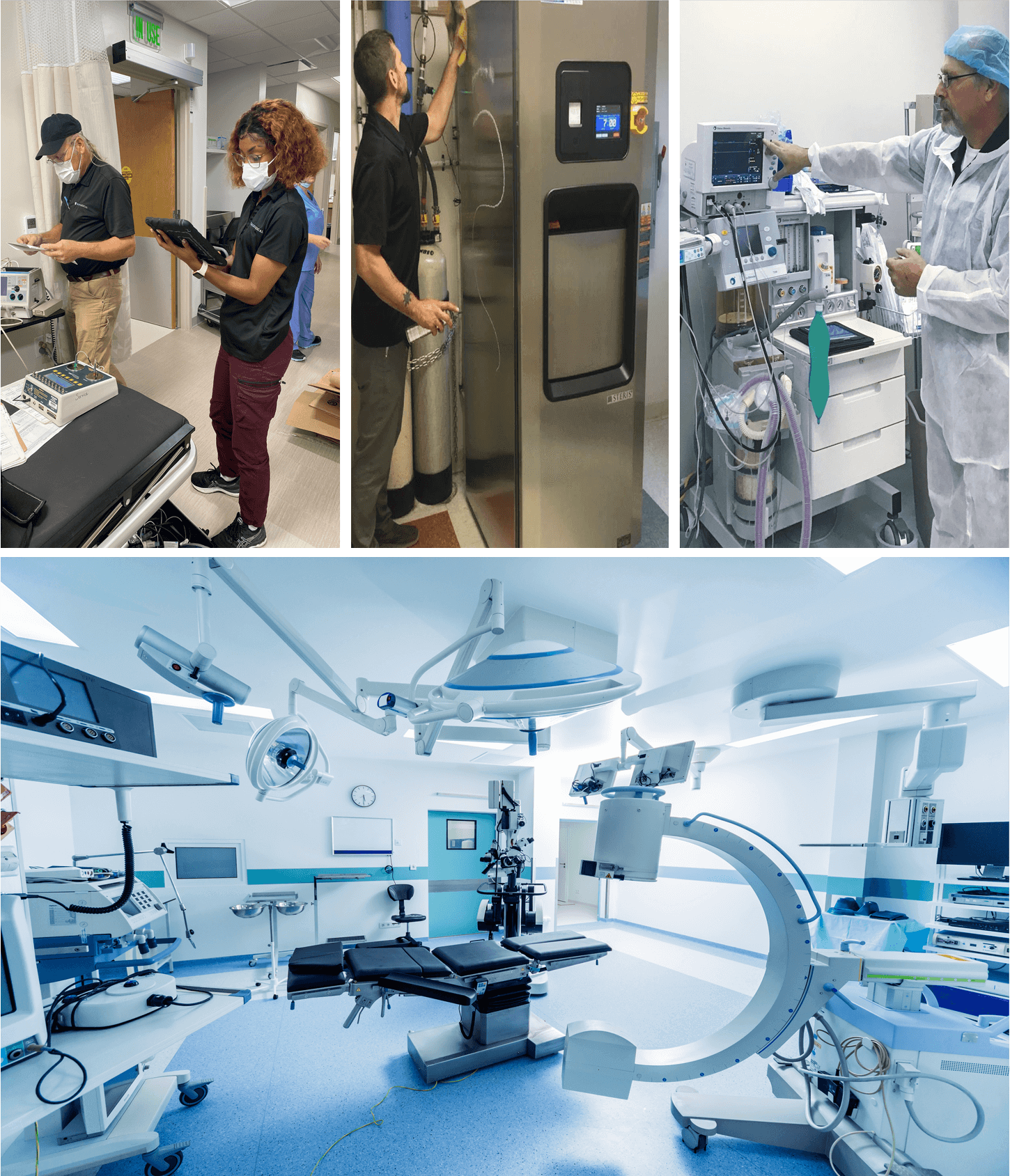
Attention all healthcare professionals! The countdown has begun, and we’re excited to remind you that our exclusive 10% off sale on select medical and lab equipment will end on July 31st, 2024. At Auxo Medical, we pride ourselves on providing top-notch new and refurbished medical equipment, maintenance, and repair services. This sale offers a fantastic opportunity to upgrade your facility with high-quality equipment at a reduced price.
Here’s a detailed look at the products currently available at a 10% discount:
Featured Sale Items
UMF Power Exam Hi-Lo Table 5060
The UMF 5060 procedure table enhances patient comfort and provider efficiency. It features a power base for height adjustment, a power backrest, and a two-function hand control. The ultra-comfort seamless upholstery simplifies cleaning and maintenance, making this table ideal for various medical examinations and procedures.
Stryker 1501 Renaissance Series Stretcher with IV Pole
This refurbished stretcher is a versatile solution for patient transport. The inclusion of an IV pole adds practicality, making it easier to manage intravenous treatments during transport. Known for its durability and ease of use, the Stryker 1501 is a staple in emergency rooms, surgical centers, and hospitals.
Mac PT-1000 Transport Stretcher (Refurbished)
The MAC PT-1000 stretcher facilitates easy and comfortable patient transfer, with a weight capacity of up to 550 lbs. Perfect for accommodating a wide range of patients, its sturdy design and user-friendly features make it an essential piece of equipment in any healthcare setting.
Edan IM70 Patient Monitor (Refurbished)
The Edan iM70 monitor meets modern clinical needs with accurate and reliable monitoring of vital signs. It offers comprehensive capabilities, including ECG, SpO2, and NIBP. Its intuitive interface ensures healthcare providers can monitor patients effectively and respond promptly to changes.
Welch Allyn Spot Vital Signs LXi Monitor
The Welch Allyn Spot LXi Monitor includes advanced features like SureBP technology for accurate blood pressure measurements and the Braun ThermoScan PRO 4000 Ear Thermometer. This monitor provides quick and reliable vital signs measurements, making it invaluable for routine check-ups and emergency assessments.
Lifepak 20E Defibrillator
The LIFEPAK® 20e defibrillator/monitor combines AED and manual defibrillation capabilities, making it ideal for first responders and medical professionals. Its intuitive design and robust performance ensure reliability in both in-hospital and out-of-hospital cardiac emergencies.
Steris Amsco Model 3085 Surgical Table
The Amsco 3085 General Surgical Table is an industry standard due to its reliability and versatility. It accommodates a wide range of surgical procedures, providing optimal positioning and support for patients. Its robust construction ensures it is a long-term investment for any surgical facility.
Midmark 623 Exam Table
The Midmark 623 Barrier-Free Examination Table enhances accessibility for patients with limited mobility. Its adjustable height mechanism allows for easy patient transfers, ensuring comfort during examinations. This table is ideal for practices catering to patients with mobility challenges.
Midmark 230 Power Procedure Chair
This chair offers adjustable features, including extending stirrups and a treatment pan, making it perfect for OB/GYN exams and various procedures. Its versatile design ensures maximum comfort for patients and ease of use for healthcare providers.
Midmark 641 Procedure Chair
The Midmark 641 features a narrow patient support surface, slim back section, and tuck-away side rails, providing versatility for various medical procedures. Its ergonomic design ensures patient comfort and allows healthcare providers to work efficiently.
Gendron 1190-231 MRI Bariatric Stretcher
Designed for bariatric patient care, this stretcher is suitable for acute care, long-term care, and home care environments. It supports larger patients safely and comfortably, ensuring ease of transport.
Skytron Hercules 6701 Surgical Table
The Hercules 6701 reduces the need for multiple support accessories and simplifies surgical set-ups. It handles a wide range of procedures, offering flexibility and reliability. Its advanced features and durable construction make it essential in modern operating rooms.
GE CardioCap 5 with 5 Agent Gas Analysis
The Cardiocap/5 is a compact, all-in-one monitor for operating rooms and ambulatory surgery units. It provides comprehensive monitoring, including 5-agent gas analysis, ensuring accurate management of anesthetic gases.
Baxter Sigma Spectrum With 6.02 Software
This refurbished infusion pump reduces Adverse Drug Events, ensuring safer patient care. Its advanced software prevents medication errors, offering peace of mind to healthcare providers and patients alike.
Braun Vista Basic
This cost-effective and easy-to-use pump is ideal for alternate site clinicians and patients. The Braun Vista Basic provides consistent performance and ease of operation, making it a practical choice for various healthcare settings.
Zoll AED Plus
The Zoll AED Plus features Real CPR Help, providing real-time feedback on the quality of CPR. Its clear visual and audio prompts make it suitable for both trained and untrained responders, ensuring effective care during cardiac emergencies.
Cardiac Science Powerheart AED G3
Designed for untrained bystanders, this AED offers step-by-step instructions for life-saving interventions. Its automated features and user-friendly design make it a valuable tool for public areas where sudden cardiac arrest may occur.
Why Choose Auxo Medical?
At Auxo Medical, we’re committed to supporting your healthcare facility with the best equipment and services. Our range of new and refurbished medical equipment meets the highest standards of quality and performance. We understand the importance of reliable equipment in providing exceptional patient care and strive to offer solutions that enhance your practice’s efficiency.
In addition to sales, we provide comprehensive maintenance and repair services to keep your equipment in optimal condition. Our experienced technicians provide timely and effective support, minimizing downtime and ensuring smooth operations. Active service agreement holders receive an additional 5% off, bringing your total discount on select items to 15% off. Act fast as the option for the total of 15% off for active service agreement holders ends July 31st, 2024
Don’t miss out on these incredible deals! Visit our sale page to view the full list of discounted items and make your purchase before the sale ends on July 31st, 2024. This is a rare opportunity to acquire high-quality medical and lab equipment at reduced prices, enhancing your practice’s capabilities and ensuring you provide the best care to your patients.
For inquiries or assistance, contact us at (888) 728-8448 or visit our website. Our team is here to help you find the right equipment and provide the support you need to keep your practice running smoothly.
-
Steris Dual Center Mount vLED Surgical Light
The Steris Dual Center Mount Harmony vLED Surgical Lighting System is a modular and configurable solution designed to provide high-quality illumination for a wide range of surgical and diagnostic applications. With a maximum central illuminance of 160,000 lux, a fixed… -
Steris Harmony LA 585 LED Dual Head OR Lights
The Steris Harmony LED 585 surgical lighting and visualization system is engineered to enhance surgical precision and patient outcomes. Its high-performance optics deliver exceptional surgical site illumination with brighter, whiter light, superior color rendition, and virtually shadow-free visibility thanks to… -
Philips Heartstart FRX AED w/ Wall Mount Box
The Philips HeartStart FRx AED is a state-of-the-art defibrillator, notable for its durability and user-friendly design. Backed by a 1-year manufacturer's warranty, this model uniquely offers an optional infant/child key, enabling the use of adult pads on pediatric patients. Lightweight… -
Verathon GlideScope Monitor with Baton
Original price was: $4,975.00.$4,726.25Current price is: $4,726.25. The Verathon GlideScope Monitor (Model: 0570-0338) with Baton (Model: 0570-0307) is a portable video laryngoscopy system designed to provide a consistently clear, real-time view of the airway, enhancing first-pass intubation success and patient safety. The system features a high-resolution 6.4-inch… -
Welch Allyn SSM Vital Signs Monitor
The Welch Allyn SSM 300 Series Vital Sign Monitor is a versatile and reliable device designed to meet the diverse needs of healthcare providers. Equipped with features such as noninvasive blood pressure (NIBP) measurement, pulse rate monitoring, and mean arterial… -
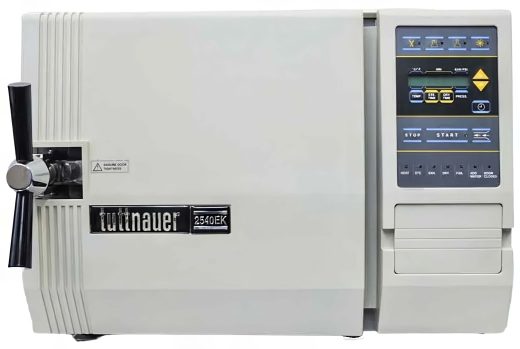
Tuttnuaer 2540EK Kwiklave Electronic Autoclave (Refurbished)
The Tuttnauer 2540EK Kwiklave Electronic Autoclave, available in a refurbished model, is a versatile and efficient sterilization device ideal for various medical and laboratory settings. It offers four distinct programs—Unwrapped, Wrapped, Liquids, and a Drying cycle—facilitating comprehensive sterilization processes. Its… -
Midmark Ritter 255 Floor Stand Light
The Midmark Ritter 255 Floor Stand Light is designed to deliver superior, white, shadow-free illumination, ensuring safety and coolness to the touch. The innovative yoke design allows for smooth and effortless maneuverability, making it easy to position exactly where needed.… -
Midmark Ritter 355 Floor Stand Light
The Midmark Ritter 355 Single Procedure Light, a perfect blend of quality and affordability tailored to meet the needs of medical professionals. This light is meticulously counterbalanced, ensuring precise positioning without any drifting, which facilitates accurate procedures. With its 4,200… -
Infinium ClearVue™ VLXL Video Laryngoscope
The Infinium® ClearVue™ VLXL video laryngoscope adopts state-of-the-art image technology and possesses the advantage of a 2.0-megapixel full view camera with 8-inch high-resolution monitor. The ClearVue™ features a rechargeable li-ion battery for mobile use. The HD optics offer a unique… -
GE Dash 4000 Patient Monitor W/ CO2
The GE Dash 4000 Patient Monitor with CO2 capabilities is a comprehensive and versatile medical device designed to meet the diverse monitoring needs of healthcare professionals. Featuring a 10.4-inch screen, this full-featured monitor provides clear and detailed displays of vital… -
ClearVue VL3R™ Reusable Video Laryngoscope
The Infinium ClearVue ™ video laryngoscope adopts state-of-the-art image technology and possesses the advantage of a 2.0-megapixel full view camera with 4-inch high-resolution monitor. The ClearVue™ features a rechargeable Li-ion battery for extended use. The HD screen offers a unique… -
Edan IM70 Patient Monitor (Refurbished)
Embedded with the latest improved designs, iM70 is meant to add splendors to the i Series portfolio and answer for the latest clinical requirements across the applications from general cares to anesthesia monitoring, while keeping connected to hospital systems in… -
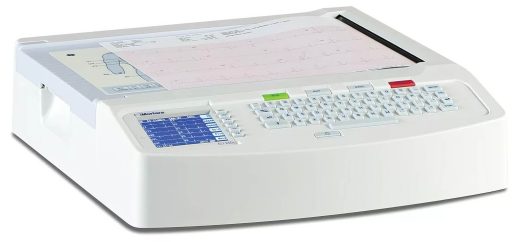
Mortara ELI 250 ECG Machine
Compact and lightweight, the ELI 250c Electrocardiograph provides comprehensive functionality in an easy-to-use, portable device. Multiple connectivity options ensure patient data transfers easily from the ECG to the location of your choice. Experience the benefits of bidirectional communication via internal… -
Mindray Passport V with CO2
Passport V is built on a solid foundation of experience and knowledge. It follows a proven approach to acquisition and presentation of patient data, thereby delivering impressive reliability and performance. Enhanced capability, more optional features and extraordinary value make Passport… -
Steris Caviwave Single Chamber Ultrasonic Cleaner 15 Gal
• Cleaning frequency of 132kHz that more than triples the commonly used 40kHz • Toe touch cycle start • Automatic chemistry injection • Automatically cleans, flushes, lubricates, and dries depending on unit configuration* • Flush ports allow tank solution reach… -
Tuttnauer EZ10k 220V Autoclave
The Tuttnauer EZ10k 220V Autoclave is a cutting-edge sterilization tool renowned for its efficiency and reliability in medical and laboratory settings. Designed with rapid cycle times, it features a fully automatic, user-friendly interface, making it ideal for high-demand environments where… -
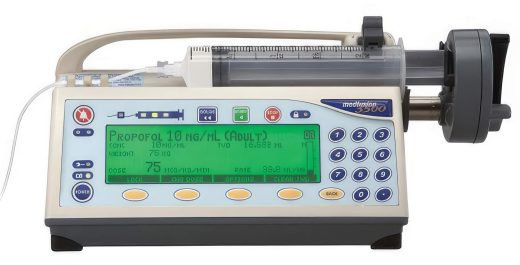
Medfusion 3500 Syringe Pump with Version 5 Software
Original price was: $1,795.00.$1,705.25Current price is: $1,705.25. The Medfusion 3500 Syringe Pump is a cutting-edge device designed to meet the needs of various departments within hospitals and medical practices. This refurbished pump features intuitive syringe detection capabilities, enhancing safety and accuracy in drug administration. Known as a… -
Welch Allyn 6000 Series Vital Signs Monitor w/ CO2
The Connex Vital Signs Monitor (VSM) 67NCXX-B is an advanced, touch screen monitor featuring bright, vivid colors with minimal knobs or buttons for ease of cleaning—perfect for hospital general care floors and for surgery centers and other ambulatory care offices.… -
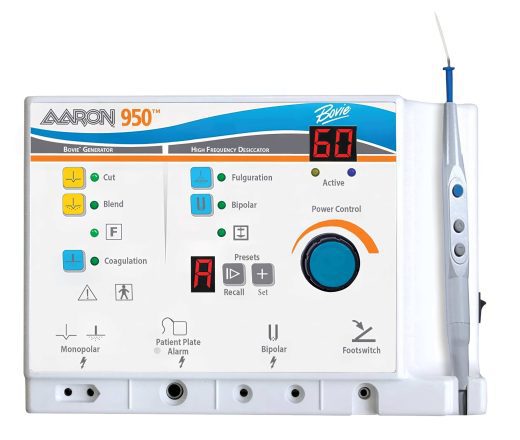
Aaron Bovie 950 High Frequency Generator
The Aaron Bovie 950 High Frequency Generator is a versatile and comprehensive electrosurgical unit designed for precision in medical procedures. This state-of-the-art generator comes equipped with a variety of components, including a power cord, a reusable handpiece, and a set… -
Steris Caviwave Rinsing and Drying Ultrasonic Cleaner
The refurbished Steris Caviwave Rinsing and Drying Ultrasonic Cleaner is a state-of-the-art cleaning system designed to deliver superior performance in medical and laboratory settings. Operating at a cleaning frequency of 132kHz, it significantly surpasses the standard 40kHz frequency, ensuring thorough… -
GE Dash 4000 Patient Monitor
The GE Dash 4000 is a comprehensive patient monitoring system designed to deliver accurate and reliable vital measurements in various clinical settings. Featuring a 10.4" screen, this full-featured monitor provides clear and concise data visualization for ease of use. Equipped… -
Gendron 1190-231 Bariatric Stretcher
Gendron develops, designs, and manufactures bariatric patient care products for acute care, long-term care, home care, and rehabilitation environments. The Gendron 1190-231 has a patient weight capacity of up to 1000 pounds and a litter top usable patient surface that… -
Hausted 5E8 Power Eye stretcher
The 5E8 is a multi-position stretcher intended for treatment, transport, or recovery of a patient. With the uniquely designed articulating head section, this unit can be used for specialty procedures which require precision head positioning, such as ophthalmology, plastic surgery,… -
Hill-Rom Transtar 8010 Eye Stretcher
Ideal for eye surgery, the Hill-Rom Surgical Stretcher (also referred to as an eye stretcher) offers outstanding mobility, functionality and quality. A surgical rail allows for easy attachment of gas delivery and drape support devices, PACU extenders and arm boards,… -
Baxter Sigma Spectrum Infusion Pump With 6.02 Software
Original price was: $995.00.$945.25Current price is: $945.25. The Baxter Sigma Spectrum Infusion Pump with 6.02 Software is a compact, user-friendly, patient-centered infusion device designed to enhance safety and efficiency in clinical settings. Equipped with Baxter's Dose Error Reduction Software (DERS), it significantly helps prevent pump-related medication errors… -
Alaris Medley 8100 Infusion Pump
Original price was: $995.00.$945.25Current price is: $945.25. The Alaris Medley 8100 Infusion Pump Module is a high-capacity, large-volume infusion device designed to seamlessly integrate into the modular Alaris System, operating in conjunction with the Alaris PC Point of Care Unit (Models 8000 or 8015). Compact and lightweight,… -
Alaris Medley 8015 Point of Care Module
Original price was: $819.00.$778.05Current price is: $778.05. The Alaris Medley 8015 Point of Care Module is a versatile, modular infusion and monitoring system designed for adult, pediatric, and neonatal care, providing clinicians with a unified interface for programming and managing multiple channels simultaneously. This compact unit, weighing… -
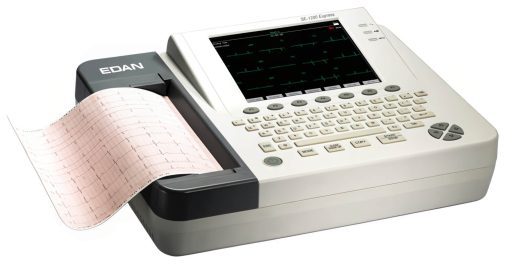
Edan SE-1200 and SE-1200 Express ECG
Excellent cost performance with built-in high-resolution thermal printer. You can record 12 ECG traces on A4 size and US Letter-size paper. [vc_btn title="Edan SE-1200 Brochure" style="flat" shape="square" link="url:/wp-content/uploads/2017/06/Edan-SE-1200-ECG-Auxo-Brochure.pdf ||target: _blank|" css=".vc_custom_1479498791367{margin-left: 5px !important;padding-right: 0px !important;padding-left: 0px !important;}"] [vc_btn title="Edan SE-1200…




















































 Our services include:
Our services include:



 What are Steris V-Pro Sterilizers?
What are Steris V-Pro Sterilizers?
