Need a Scrub Station? Auxo Medical has it.
The Importance of a Reliable Scrub Station in Healthcare
In the healthcare industry, maintaining a sterile environment is crucial. A reliable and efficient scrub station is essential for ensuring cleanliness among surgical staff before they enter the operating room. Whether you’re setting up a new facility or upgrading an existing one, a high-quality scrub station is a must. Auxo Medical offers a range of scrub stations designed to meet the strict requirements of healthcare facilities. In this article, we’ll explore the benefits of choosing Auxo Medical for your scrub station needs and how our products can enhance your facility’s efficiency and hygiene.
Why a High-Quality Scrub Station Matters
A scrub station is more than just a sink; it plays a vital role in preventing infections and contamination. The right scrub station helps ensure compliance with health and safety regulations, making it an essential piece of equipment in any medical setting.
Key Features of a High-Quality Scrub Station
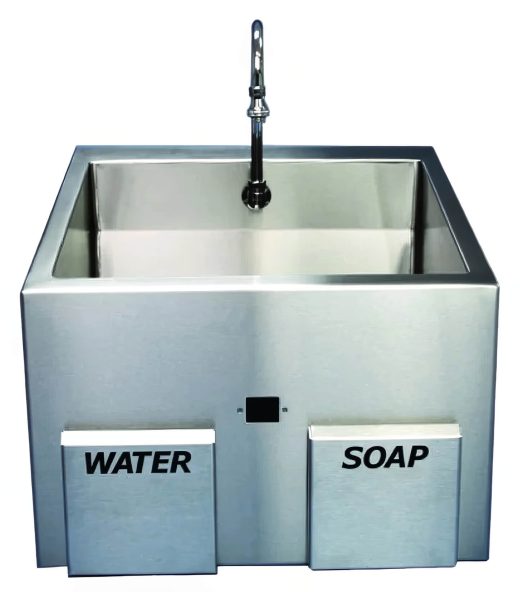
- Hands-Free Operation: To prevent cross-contamination, look for scrub stations with foot pedals or sensor-activated faucets.
- Durable Materials: Choose scrub stations made from stainless steel, which is easy to clean and withstands frequent use.
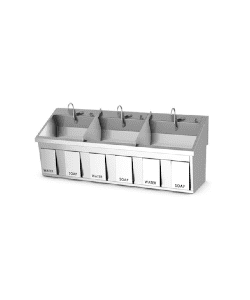
- Adequate Space: A well-designed scrub station should accommodate multiple users, allowing surgical teams to scrub in efficiently.
- Integrated Soap Dispensers: Built-in soap dispensers and brush holders ensure that all necessary supplies are readily available.
For more details on our scrub stations, visit our online catalog.
Why Choose Auxo Medical?
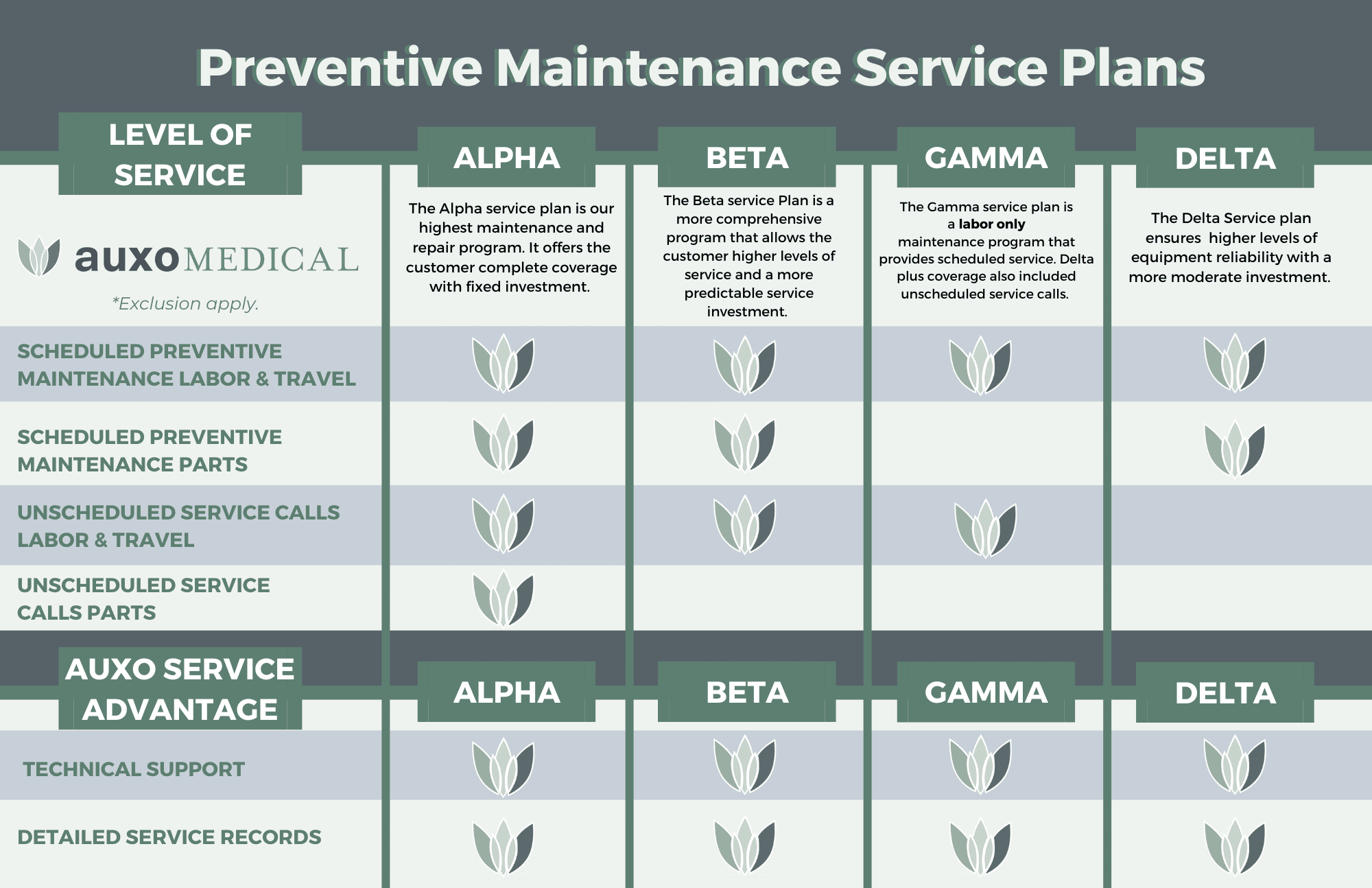
Auxo Medical is a trusted provider of medical equipment, offering a wide range of high-quality products for healthcare facilities. Here are a few reasons to choose us for your scrub station needs:
Superior Quality and Durability
Our scrub stations are made from high-quality stainless steel, ensuring they are durable and easy to clean. This construction allows them to withstand the demands of a busy healthcare environment.
Competitive Pricing
We believe that high-quality medical equipment should be accessible to all. Auxo Medical offers competitive pricing on our scrub stations, providing great value without compromising quality.
Expert Support and Installation
Our team of experts is here to assist you throughout the process. From selecting the right scrub station to installation and ongoing maintenance, we offer comprehensive support to ensure your scrub station operates efficiently.
Enhancing Efficiency and Hygiene with Auxo Medical Scrub Stations
Investing in a high-quality scrub station from Auxo Medical can significantly improve the efficiency and hygiene of your facility. Here are some benefits:
- Improved Workflow: Our scrub stations accommodate multiple users, allowing surgical teams to scrub in quickly and efficiently. This streamlined workflow helps reduce delays.
- Enhanced Hygiene: Features like hands-free operation and integrated soap dispensers maintain a sterile environment, reducing infection risks and ensuring regulatory compliance.
- Easy Maintenance: Made from durable stainless steel, our scrub stations are simple to clean and maintain, ensuring reliable performance for years.
Order Your Scrub Sinks from Auxo Medical
A high-quality scrub station is vital for maintaining a sterile environment and ensuring your facility operates efficiently. Auxo Medical offers a range of scrub stations tailored to the needs of healthcare facilities, providing superior quality, customization options, competitive pricing, and expert support. By choosing Auxo Medical, you enhance both the efficiency and hygiene of your facility, ensuring optimal patient care.
Take Action with Auxo Medical
Investing in the right scrub station is essential for maintaining a sterile environment. At Auxo Medical, we offer high-quality scrub stations designed for healthcare facilities. Don’t compromise on quality—explore our range and find the perfect solution for your needs. For more information, view our online catalog or schedule a consultation by visiting our contact page or calling (888) 728-8448.
FAQ
- What materials are Auxo Medical scrub stations made from?
- Our scrub stations are constructed from high-quality stainless steel, ensuring durability and easy cleaning.
- How does hands-free operation work on Auxo Medical scrub stations?
- Our scrub stations feature hands-free operation through foot pedals or sensor-activated faucets, minimizing cross-contamination.
- What support does Auxo Medical provide for scrub station installation?
- We offer comprehensive support, including expert guidance on selecting the right station, professional installation, and maintenance options.
- How can I schedule a consultation with Auxo Medical?
- To schedule a consultation, view our online catalog and request a quote, or contact us directly at (888) 728-8448. Our team will help develop a customized plan for your facility.
Thank you for learning about how Auxo Medical can meet your scrub station needs. We are dedicated to providing healthcare professionals with the highest quality products and services for optimal patient care and operational efficiency. For more information, please view our online catalog or contact us directly at (888) 728-8448.
-
SS Series Dual Bay Surgical Scrub Sink with Infrared Operated Water & Soap
The SS Series Dual Bay Surgical Scrub Sink is equipped with infrared-operated water and soap dispensing systems. Standard features include a deep sloping basin and an adjustable thermostatic controlled pressure regulating mixing valve for each station. Maintenance is simplified with… -
Dual Bay Economy Sink with Manual Knee Operated Water
The Dual Bay Economy Sink with Manual Knee Operated Water, part of the ES Series, offers a practical and hygienic handwashing solution. The ES47 model features a 47-inch wide sink with a deep, sloping basin designed for effective scrubbing. This… -
Steris Manual Dual Bay Flexmatic Scrub Sink
Dual bay Flexmatic scrub station without timer or water control sensor. Each unit is constructed of welded 16 gauge stainless steel with a matte finish for easy cleaning and low maintenance. The built-in thermostatically controlled mixing valve provides optimum water… -
Dual Bay Flexematic Scrubsink, IR
Dual bay Flexmatic scrub station without timer or water control sensor. Each unit is constructed of welded 16 gauge stainless steel with a matter finish for easy cleaning and low maintenance. The built-in thermostatically controlled mixing valve provides optimum water… -
SS Series Dual Bay Surgical Scrub Sink W/ Knee Operated Water & Soap
The SS-Series Surgical Scrub Sinks were developed to answer space and economical constraints where needed. These sinks have smaller outside dimensions but still maintain a deep basin to allow for proper scrubbing. [vc_btn title="Download Brochure" style="flat" shape="square" link="url:/wp-content/uploads/2017/06/Dual-Bay-Surgical-Scrub-Sink-W-Knee-Operated-Auxo-Brochure.pdf ||target: _blank|" css=".vc_custom_1479498791367{margin-left: 5px… -
ES Series Dual Bay Economy Sink W/ Infrared Operated Water
The ES-Series Surgical Scrub Sinks were developed to answer space and economical constraints where needed. These sinks have smaller outside dimensions but still maintain a deep basin to allow for proper scrubbing. [vc_btn title="Download Brochure" style="flat" shape="square" link="url:/wp-content/uploads/2017/06/Dual-Bay-Economy-Sink-W-IR-Operated-Water-Auxo-Brochure.pdf ||target: _blank|" css=".vc_custom_1479498791367{margin-left: 5px… -
SS Series Single Bay Surgical Scrub Sink With Knee Operated Water & Soap
The SS Series Single Bay Surgical Scrub Sink offers a blend of quality and affordability, making it an excellent choice for upgrading or equipping surgical facilities. This sink features knee-operated water and soap dispensing, promoting hygienic, hands-free operation. Standard features… -
Steris Amsco Flexmatic Single Bay Scrub Station
Designed in accordance with Underwriters Laboratories standards to meet all of your scrub sink needs, Amsco®Flexmatic® Scrub Sinks have stood the test of time. These durable sinks feature continuous welded compartments and coved corners constructed entirely of stainless steel for easy…











 Product Overview
Product Overview Product Overview
Product Overview Product Overview
Product Overview










 1. Ensuring Patient Safety
1. Ensuring Patient Safety